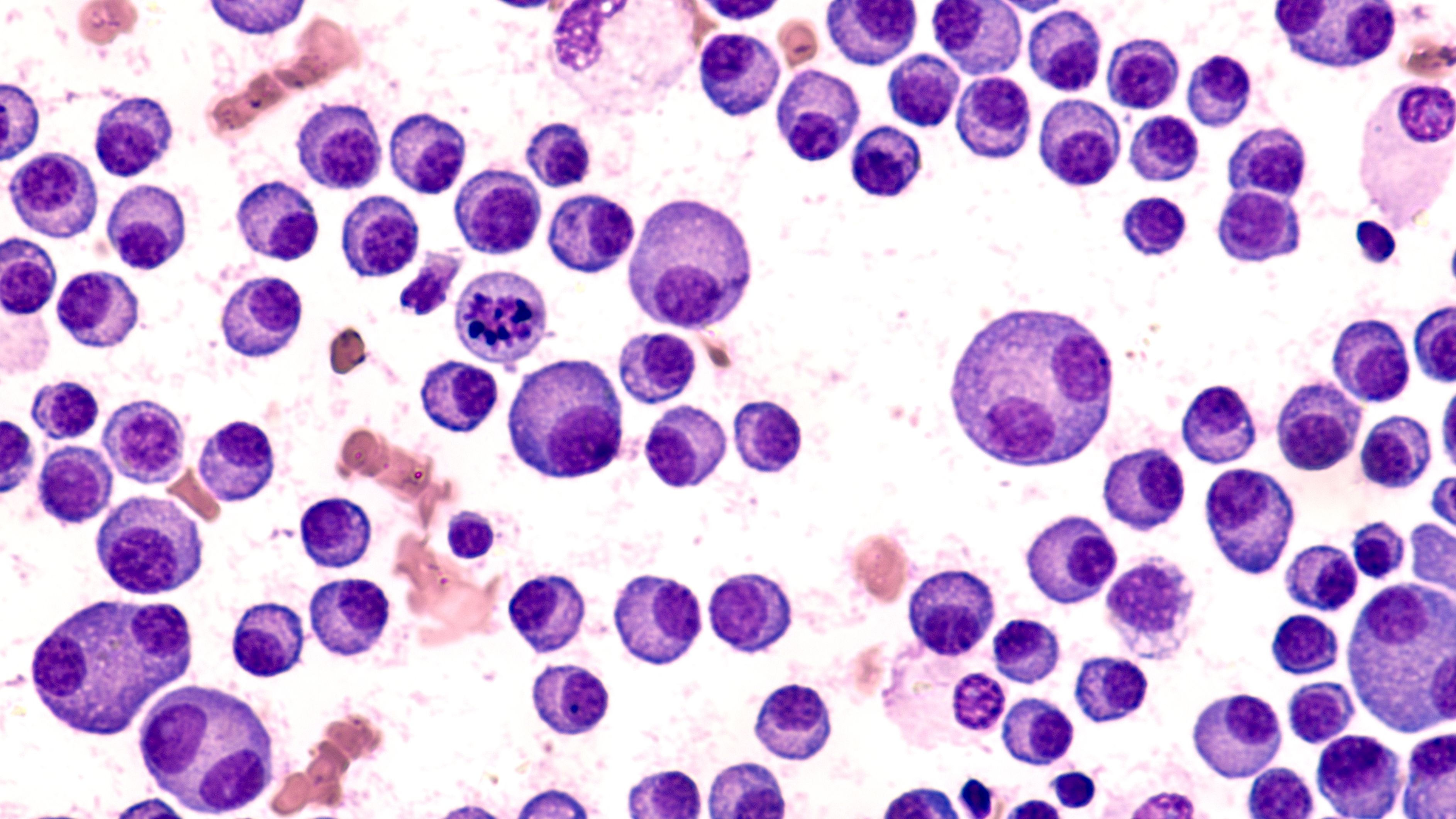
Image Credit: © Murrstock – stock.adobe.com
We presented an initial review of quality tolerance limit (QTL) adoption trends in the March 2023 issue of Applied Clinical Trials, based on information compiled from the CluePoints RBQM platform through the end of 2022. In this article, we present an updated view that includes QTL adoption data through the end of 2023, comprising a total of 631 QTLs created in 254 studies since 2019. We also take a closer look at the types of QTLs that organizations are choosing to implement.
We reported in the previous article that QTLs were implemented in 37.7% of new studies in 2022. This increased to 58.1% in 2023, which confirms that the adoption of QTLs has continued to grow rapidly (see Figure 1). The median number of QTLs per study remained at two, as it was in our previous article.

Additionally, we provided a distribution of the QTLs across three general categories as follows. Results remain very consistent with the updated data.
- Compliance: 55.8% through 2022, up to 62.3% through 2023.
- Enrollment and retention: 32.5% through 2022, down to 29.2% through 2023.
- Safety: 11.3% through 2022, down to 8.5% through 2023.
This year, we have additionally assigned a more specific QTL type for every QTL parameter implemented on the platform, so that we can assess which types are the most commonly used. QTLs for “missed assessment rate” are the most common, occurring in 57.5% of all studies having QTLs. This is followed by “enrolled but ineligible rate” (25.6%) and “early termination rate” (23.6%).
Our data indicated that a strong majority of QTLs being implemented thus far are focused on risks related to data reliability, and more specifically the risk of not having sufficient data to support evaluation of study endpoints. The top four QTL types are arguably in this category, assessing the loss or attrition of evaluable data (or patients) in some form. The fifth QTL type, “safety event of interest rate,” appears in 14.6% of studies using QTLs and focuses risks related to patient safety. The QTL type, “lost to follow-up rate” (14.2% of studies), may have implications for both data reliability and patient safety.
Steve Young, Chief Scientific Officer, CluePoints; Sylviane de Viron, Data and Knowledge Manager, CluePoints